Across the Ontario health care system, there is developing interest in designing care approaches that better address the needs of older adults (individuals aged 65+) living with multiple, and often interacting, complex and chronic health conditions, sometimes referred to as frailty. The development of this statement has been led by members of the Ontario Collaborative for Aging Well (OCAW), a grass-roots group of local, regional and provincial partners who work with older adults living with or at risk of frailty. Arising out of demand for support to manage the care of individuals living with frailty emerging from Ontario Health Teams (OHTs), OCAW brings together 25 organizations representing: age friendly communities; caregivers; dementia experts; francophone planners; mental health and addictions experts; older adults; rehabilitative experts; research and academic institutes; OHTs (inclusive of primary care); and specialized geriatric services[1].
OCAW recognizes the growing international frailty-related evidence as central to informing high quality care for older adults living with complex and chronic conditions. At the same time, OCAW acknowledges that the term “frailty” is neither consistently defined nor popular with older adults. This statement is intended to provide clarity about concepts related to complexity and frailty as they relate to the planning and delivery of care required by older adults in Ontario.
Drawing from ecological theory, systems theory, older adult[2] and clinician experience, and philosophical stances evident in international initiatives such as Age Friendly Communities[3], OCAW recommends that concepts such as complexity and frailty, must include the physical, cognitive, mental, and social health of older adults and their care partners and the interaction and integration of these domains.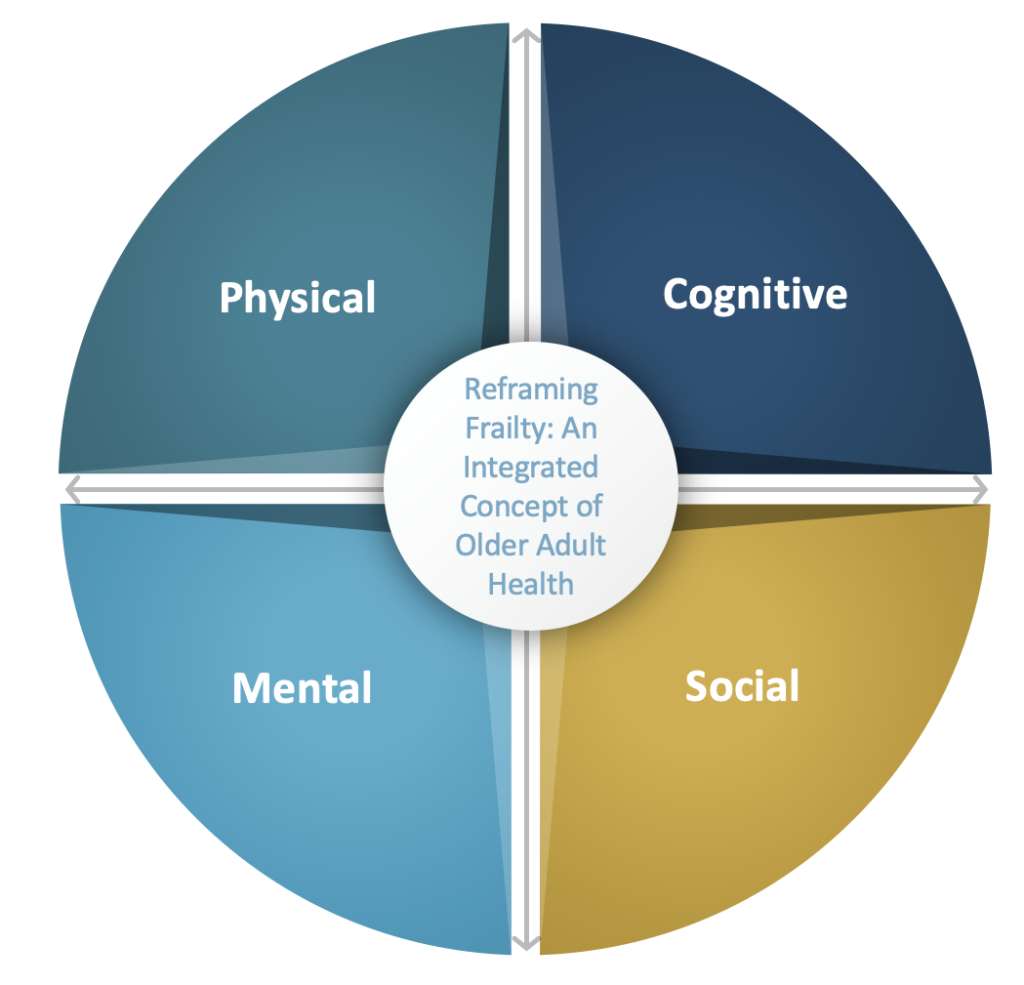
Considered this way, an older adult may simultaneously demonstrate some or all of: a change or reduction in function or decline from relatively minor illness (physical)[4]; changes in thinking or memory that may also impact function (cognition)[5],[6],[7]; changes in mood (e.g. depression[8],[9],[10],[11]) or psychological well-being (mental health[12]); and/or a limited or inconsistent support network5, loneliness and social isolation, housing precarity, or food insecurity among other concerns, as well as the impacts of structural ageism, institutional racism and other forms of discrimination (social health). Supporting older adults with complex needs requires holistic, coordinated and integrated approaches to promote independence and quality of life, and prevent adverse events (e.g. falls, institutionalization).
Labels and Language – A Caution
Older adults have expressed that being associated with the term ‘frailty’ is undesirable. They describe that being called frail impacts their sense of self, and lowers the expectations others have of them, and that they have of themselves. This can mean that older adults may not be offered or do not ask for what they require to address illness or health challenges. This may also mean that more disruptive and costly health care options become necessary when problems contributing to complex health conditions go unaddressed. Older adults report that the term frailty is associated with health professionals “giving up on us”[13].
There is value in aligning service planning and design with relevant evidence, such as frailty-specific research, and related screening and assessment tools. At the same time, applying labels to people is a dangerous practice with unintended consequences. Frailty is not a diagnosis, but rather describes a constellation of complex health and social conditions, many of which are amenable to mitigation. In some jurisdictions the language of enhancing ‘vitality’ is taking hold[14], as is the concept of resilience[15]. OCAW applauds this re-framing. Thus OCAW urges caution in the application of the term frailty and recommends that: person first language always be used (i.e. an older adult living with or experiencing complex health conditions); the dynamic nature of complexity or frailty be recognized; and that appropriate screening, assessment, diagnosis, treatments and interventions, and follow-up be offered to older individuals demonstrating changes in physical, cognitive, mental and social health.
Version May 26, 2022
Further Learning
Ontario
Regional Geriatric Programs (Specialized Geriatric Services)
Geriatric Essentials E-Learning (Frailty and other modules)
https://geriatricessentialselearning.ca/ (Free – Registration Required)
Canada
Canadian Frailty Network
Frailty: Assessment, Mitigation & Prevention Module
https://www.cfn-nce.ca/training/frailty-module/ (Free – Registration Required)
Contact about this statement: info@rgpo.ca
References
[1] Geriatric services include geriatric medicine, geriatric psychiatry, seniors’ mental health, care of the elderly and interprofessional geriatrics teams
[2] Martin, D., Long, O., & Kessler, L. (2019). https://doi.org/10.1080/02763893.2019.1593280
[3] Lehning, A., & Greenfield, E. (2017). https://doi.org/10.1080/02763893.2017.1309937
[4] Canadian Frailty Network https://www.cfn-nce.ca/frailty-matters/what-is-frailty/
[5] Rivan et al. (2021). https://bmcgeriatr.biomedcentral.com/articles/10.1186/s12877-021-02525-y
[6] Ellwood et al. (2021). https://doi.org/10.1177/01640275211045603
[7] Sargent et al. (2018). http://doi.org/10.1016/j.arr.2018.08.001
[8] Brown et al. (2020). https://doi.org/10.1016/j.jagp.2019.10.005
[9] Lohman et al. (2016). https://doi.org/10.1093/geronb/gbu180
[10] Frost et al. (2021). https://doi.org/10.1080/13607863.2019.1647132
[11] Voshar et al. (2021). https://doi.org/10.1002/gps.5588
[12] WHO (2018). https://www.who.int/news-room/fact-sheets/detail/mental-health-strengthening-our-response
[13] Provincial Geriatrics Leadership Ontario Older Adult and Care Partner Advisory Council
[14] See Alberta Health Services various references
[15] RCA and PGLO. (2021). Rehabilitative Care for Older Adults Living With/At Risk of Frailty: From Frailty to Resilience. http://rehabcarealliance.ca/uploads/File/Initiatives_and_Toolkits/Frail_Seniors/Rehab_for_Older_Adults_Living_with_Frailty_Framework.pdf