A Resource for Patients and Families – Developed by Older Adults and Care Partners.
This resource document, prepared by the Provincial Geriatrics Leadership Ontario (PGLO) Older Adult and Care Partner Advisory Council, helps to explain what a comprehensive geriatric assessment is and how you might best prepare for this special type of clinical appointment.
To download this resource, click the button below.
[For a French version of this tool, click right.]
More information about the Comprehensive Geriatric Assessment:
A Comprehensive Geriatric Assessment (CGA) is a form of comprehensive assessment that is best suited to older adults living with complex and/or multiple co-morbid conditions such as dementia, frailty, seniors’ mental health or a combination of these and other conditions. Several meta-analyses have identified that CGA increases the likelihood of detecting cognitive impairment and improving quality of care for people living with dementia and other common geriatric conditions (e.g. falls, urinary incontinence, etc.)[1].
The CGA may be carried out in different health care settings including acute care, primary care and community-based care. In acute care, CGAs carried out by interprofessional teams of knowledgeable actors (e.g. geriatric services) have reduced mortality, length of stay, and long-term care home admissions for up to one year post discharge, and improved functional status, and quality of life[1]. A recent systematic review concluded that CGA significantly increased independence and reduced mortality for hospitalized older adults with frailty[2].
Interprofessional CGA-based community programs that support ongoing treatment and uptake of recommendations have been shown to reduce mortality, functional decline and admission to long-term care[1]. Home-based CGA has also been shown to improve functional status and patient satisfaction, increase health related quality of life and reduce mortality and hospitalization[3]. In emergency departments (ED), a targeted geriatric assessment, drawing from specific domains and modalities of CGA, is usually recommended as an alternative to a full CGA, given the urgency of presenting problems, availability of interprofessional team members, and the overall ED context.
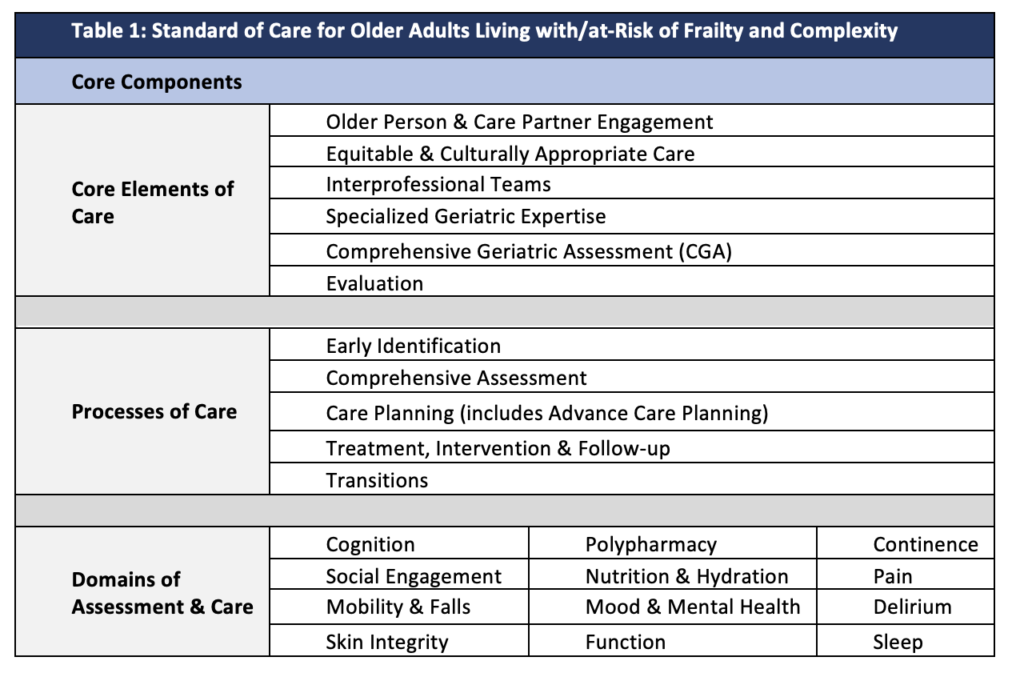
Assessment activities included in the CGA generally occur in the context of other clinical activities that have been accepted as the standard of care for older adults living with/at-risk of frailty and complexity in Ontario [4].
Table 1 illustrates the core elements of care, key processes and domains of assessment and care included in the CGA and related follow-up activities, including treatments and recommendations.
References:
[1] Pilotto, A. et al. (2016). Three decades of comprehensive geriatric assessment: Evidence coming from different healthcare settings and specific clinical conditions. Journal of the American Medical Directors Association. http://dx.doi.org/10.1016/j.jamda.2016.11.004
[2] Xu et al. (2024). The effectiveness of comprehensive geriatric assessment for older adults with frailty in hospital settings. A systematic review and meta-analysis. International journal of nursing studies. 159, 10489. 10.1016/j.ijnurstu.2024.104849
[3] Hayes et al. (2025). Home-based comprehensive geriatric assessment for community dwelling at-risk, frail older adults: a systematic review and meta-analysis.
[4] Kay, K., Hawkins, S., Day, A., Briscoe, M., Daly, D. and Wong, K., (2017). A competency framework for interprofessional comprehensive geriatric assessment. Regional Geriatric Programs of Ontario. https://geriatricsontario.ca/wp-content/uploads/2019/03/A-Competency-Framework.pdf. Acknowledgements: D. Corsi.